- 13.6% of American Indians/Alaskan Native adults
- 12.1% of non-Hispanic Black adults
- 11.7% of Hispanic adults
- 9.1% of Asian American adults
- 6.9% of non-Hispanic White adults
Despite having a higher likelihood of developing diabetes and associated complications, minority patients are less likely to receive preventative care. Gaps in healthcare access and diabetes prevention include regular A1c testing, annual cholesterol screenings, eye examinations, and more.
Even when non-white patients follow care guidelines, mistakes in accuracy can occur, such as in A1C tests. A study in the National Library of Medicine highlights how disparities in A1C readings can lead to misdiagnoses and ineffective treatment plans—particularly impacting underserved communities.
Populations with the Highest Rates of Hemoglobin Variants in the U.S.
| Hemoglobin Variant | Prevalence in the U.S. |
|---|---|
| Hemoglobin S (HbS) | |
| Hemoglobin C (HbC) | |
| Hemoglobin E (HbE) |
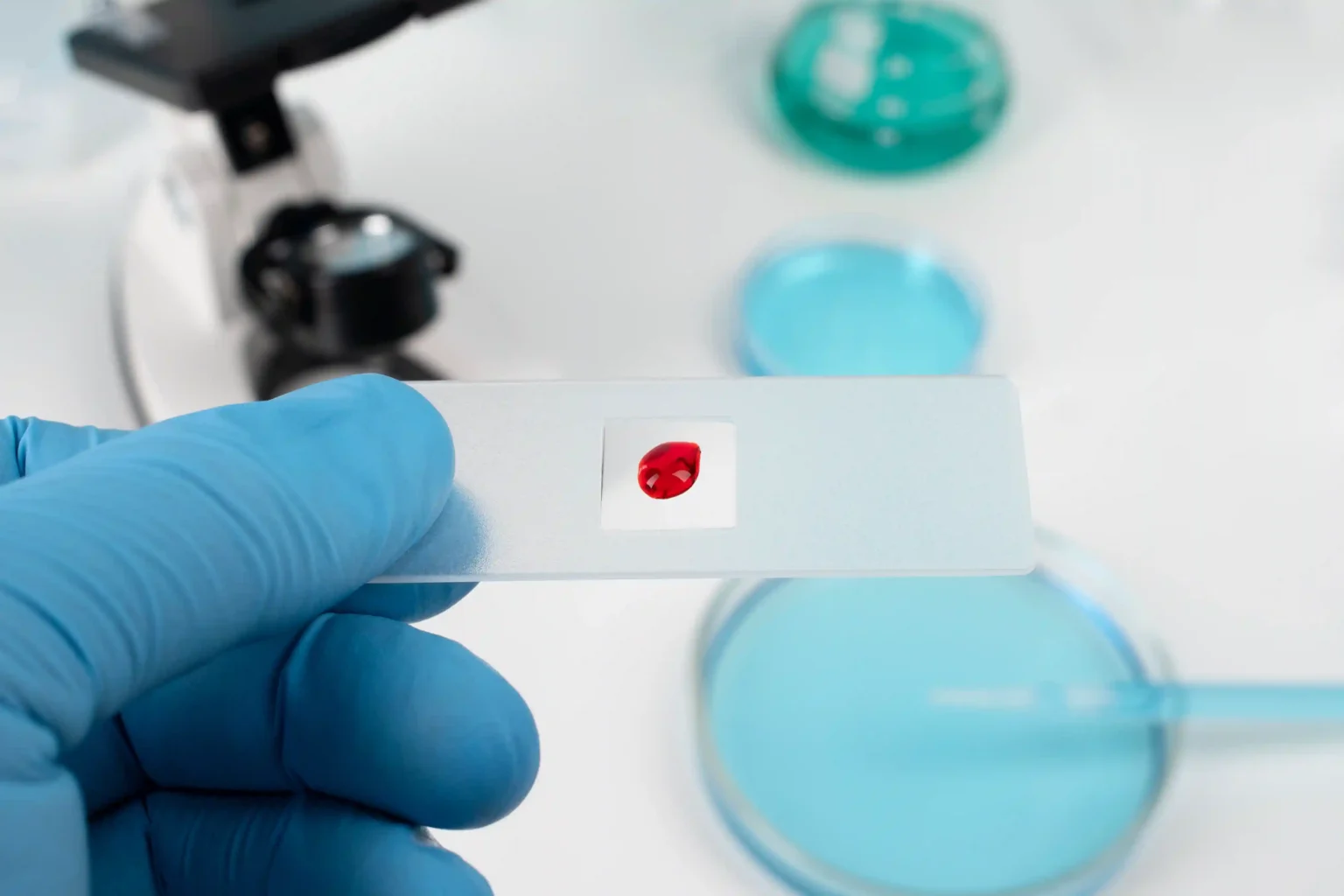
Orange Biomed’s New A1C Testing Method: Key Commitment to Diversity
OBM rapid A1c is a new, more accurate method of testing, anticipated to be released soon. The company stands behind our commitment to racial diversity. Learn more about OBM rapid A1c here.
Sources:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3557948
- https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/diabetes/sickle-cell-trait-hemoglobinopathies-diabetes
- https://www.mlo-online.com/disease/diabetes/article/21203094/the-role-of-race-and-ethnicity-in-variant-hemoglobin-traits
- https://www.heart.org/en/news/2021/07/13/the-challenge-of-diabetes-in-the-black-community-needs-comprehensive-solutions
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7935471
- https://diabetes.org/about-diabetes/statistics/about-diabetes